Diabetes & Hypertension Retina
Introduction
The eyes serve as windows to our health, offering insights into various systemic conditions. Among the most prevalent diseases affecting eye health are diabetes and hypertension. Both of these conditions can significantly impact the delicate structures of the retina, leading to potentially sight-threatening complications. Understanding the interplay between diabetes, hypertension, and retinal health is crucial for effective management and prevention of vision loss.
Diabetic Retinopathy :
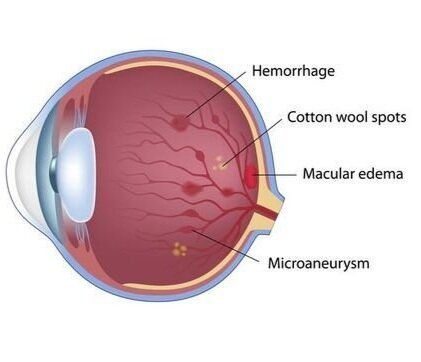
Diabetic retinopathy is a common complication of diabetes and a leading cause of blindness among working-age adults. Chronically elevated blood sugar levels can damage the small blood vessels in the retina, leading to leakage, swelling, and even abnormal growth of new blood vessels. These changes can result in vision impairment or blindness if left untreated. Early detection through regular eye exams is essential for timely intervention and prevention of irreversible damage.
The Two Stages of Diabetic Eye Disease
There are two main stages of diabetic eye disease.
NPDR (non-proliferative diabetic retinopathy)
This is the early stage of diabetic eye disease. Many people with diabetes have it.
With NPDR, tiny blood vessels leak, making the retina swell. When the macula swells, it is called macular edema. This is the most common reason why people with diabetes lose their vision.
Also with NPDR, blood vessels in the retina can close off. This is called macular ischemia. When that happens, blood cannot reach the macula. Sometimes tiny particles called exudates can form in the retina. These can affect your vision too.
If you have NPDR, your vision will be blurry.
PDR (proliferative diabetic retinopathy)
PDR is the more advanced stage of diabetic eye disease. It happens when the retina starts growing new blood vessels. This is called neovascularization. These fragile new vessels often bleed into the vitreous. If they only bleed a little, you might see a few dark floaters. If they bleed a lot, it might block all vision.
These new blood vessels can form scar tissue. Scar tissue can cause problems with the macula or lead to a detached retina.
PDR is very serious, and can steal both your central and peripheral (side) vision.
Risk factors
Anyone who has diabetes can develop diabetic retinopathy. The risk of developing the eye condition can increase as a result of :
- Having diabetes for a long time
- Poor control of your blood sugar level
- High blood pressure
- High cholesterol
- Pregnancy
- Tobacco use
- Being Black, Hispanic or Native American
Prevention
You can't always prevent diabetic retinopathy. However, regular eye exams, good control of your blood sugar and blood pressure, and early intervention for vision problems can help prevent severe vision loss.
If you have diabetes, reduce your risk of getting diabetic retinopathy by doing the following :
- Manage your diabetes. Make healthy eating and physical activity part of your daily routine. Try to get at least 150 minutes of moderate aerobic activity, such as walking, each week. Take oral diabetes medications or insulin as directed.
- Monitor your blood sugar level. You might need to check and record your blood sugar level several times a day — or more frequently if you're ill or under stress. Ask your doctor how often you need to test your blood sugar.
- Ask your doctor about a glycosylated hemoglobin test. The glycosylated hemoglobin test, or hemoglobin A1C test, reflects your average blood sugar level for the two- to three-month period before the test. For most people with diabetes, the A1C goal is to be under 7%.
- Keep your blood pressure and cholesterol under control. Eating healthy foods, exercising regularly and losing excess weight can help. Sometimes medication is needed, too.
- If you smoke or use other types of tobacco, ask your doctor to help you quit. Smoking increases your risk of various diabetes complications, including diabetic retinopathy.
- Pay attention to vision changes. Contact your eye doctor right away if your vision suddenly changes or becomes blurry, spotty or hazy.
Remember, diabetes doesn't necessarily lead to vision loss. Taking an active role in diabetes management can go a long way toward preventing complications.
Diagnosis
Diabetic retinopathy can be diagnosed through a comprehensive eye examination. Testing, with emphasis on evaluating the retina and macula, may include :
- Visual acuity measurements to evaluate your central vision.
- Refraction to determine if a new eyeglass prescription is needed (this is the whole “Which is clearer: 1 or 2?” phase of the appointment). With uncontrolled diabetes and diabetic retinopathy, your prescription may change more frequently.
- Dilation to evaluate the structure of your entire eyeball, including the retina. Yes, this is the test that includes that annoying, but painless, eye drop!
- Tonometry to measure the pressure in your eye. Sometimes this is done with that funny little puff of air on your eyeball.
If your doctor suspects diabetic retinopathy, she or he may do further testing :
- Retinal or fundus photography to get a close-up picture of the back of your eyeball.
- Optical coherence tomography to get a high-resolution, cross-sectional image of the retina to see if there is macular edema.
- Fluorescein angiography to evaluate blood flow through the retinal vessels and check for blockages and/or leakage. A yellow dye (called fluorescein) will be injected into a vein and then a camera takes photos of your retina as the dye travels throughout its blood vessels.
Management and Treatment
- Injections : Your healthcare provider injects medication, such as anti-vascular endothelial growth factor drugs or corticosteroids, into your eye. These medicines help slow down disease progression and improve vision.
- Laser surgery : Your healthcare provider uses a laser to reduce swelling in your retina and new blood vessel growth. The lasers shrink blood vessels or stop leaking.
- Vitrectomy : Your healthcare provider may recommend this outpatient eye surgery if you have cloudy vision due to leaking blood vessels. During a vitrectomy, the eye doctor makes a small incision in the eye. The provider can repair the blood vessels and remove scar tissue.
Hypertensive Retinopathy :
Hypertensive retinopathy occurs due to high blood pressure, which causes damage to the blood vessels supplying the retina. In response to elevated blood pressure, these vessels may narrow, leak fluid, or become blocked, compromising blood flow to the retina. As a result, individuals with hypertensive retinopathy may experience symptoms such as blurred vision, headaches, or even vision loss. Controlling blood pressure through lifestyle modifications and medication is crucial in preventing and managing hypertensive retinopathy.
Overlap and Complications :
It's important to note that many individuals with diabetes also have hypertension, further exacerbating the risk of retinal complications. The combination of these conditions can accelerate retinal damage, increasing the likelihood of severe vision impairment. Additionally, diabetic retinopathy and hypertensive retinopathy share common features, making it challenging to differentiate between the two based solely on clinical presentation. Therefore, comprehensive eye exams, including imaging studies, are essential for accurate diagnosis and treatment planning.
Prevention and Management :
Prevention and management strategies for diabetic and hypertensive retinopathy primarily focus on controlling underlying medical conditions. Tight glycemic control in diabetes and blood pressure management in hypertension are paramount in preventing retinal complications. Lifestyle modifications such as maintaining a healthy diet, regular exercise, and abstaining from smoking can also help mitigate the risk of retinal damage. For individuals already experiencing retinal changes, treatments such as laser therapy, intravitreal injections, or surgery may be necessary to preserve vision and prevent further deterioration.